Understanding Trauma Through the Window of Tolerance

One of the most significant markers of living with trauma is the decreased ability to not only tolerate and recover from expected and normal stress but to connect with others and engage in relationships of all kinds. The capacity to meaningfully engage socially and experience nervous system recovery is referred to as the Window of Tolerance, a phrase and idea coined by psychiatrist Daniel Siegel, and what Stephen Porges refers to as the social engagement system in polyvagal theory.
Outside the window of tolerance are hyperarousal and hypoarousal. Hyperarousal refers to the fight or flight activation of the nervous system, and hypoarousal is the nervous system’s freeze response. Someone may move out of their window of tolerance and into one of these states after experiencing or witnessing a traumatic event, enduring intense stress over a long period of time with no relief or experiencing extended loneliness and isolation. All of these can cause the threshold for stress and connection to decrease—the window narrows.
When the window is vast, there is greater tolerance and flexibility to handle various stressors and hardships and enjoy relationships. The optimal window of tolerance does not mean that there is an absence of stressors or that life is remarkably easy. The optimal zone is characterized by stress recovery and the ability to function and thrive in everyday life, however, that may look for the individual, with a sense of feeling grounded and open.
Other than engaging in meaningful, mutual relationships and an ability to recover from regular stress, there is no set measure or standard for a healthy window of tolerance because this depends on the individual. Just as everyone reacts differently to trauma, everyone will have a different window of patience, and this window will naturally widen and narrow throughout a lifetime. Noticing when the window doesn’t widen after a period of narrowing is vital when working with the nervous system.
Hyperarousal
Hyperarousal is the fight or flight response of the autonomic nervous system. The nervous system will move into this state when there is imminent danger, signaling the body to take action to secure safety. In everyday life, people can move into some aspects of this state before taking a test or having a job interview, for example, and it’s generally felt as situation-appropriate anxiety with the body recovering and returning to its window of tolerance shortly after the situation ends.
When the body remains in hyperarousal, however, this means that it is stuck in a hypervigilant state, giving someone a feeling of always being on guard or on edge.
Some symptoms of hyperarousal are:
- Excessive startle response
- Difficulty concentrating, focusing and/or making decisions
- Difficulty sleeping
- Impulsivity
- Outbursts caused by anger
- Meltdown caused by overwhelm
- Easily panicked
- Constant anxiety
- Irritability
- Avoidance of social situations and/or people
- Constant muscle tension, leading to body aches and possibly pain
- Heightened sensory sensitivity
Living with trauma can put people into a constant state of hyperarousal when there is no real threat or danger, ultimately affecting their relationships, employment and ability to function in and enjoy everyday life.
Hypoarousal
The freeze state, or hypoarousal, is a nervous system response triggered by overwhelming stress that causes the body to shut down into a frozen state. This is also called a collapsed state and can resemble depression. The freeze state is an evolutionary mammalian response to an immediate threat that causes immobilization as a survival response. Many animals go into freeze or “play dead” to survive threats, and humans are no different.
Common characteristics of hypoarousal are:
- Emotional or mental numbness
- Lack of energy
- Extreme fatigue and/or sudden fatigue
- Inability to think or respond
- Brain fog
- Dissociation
- Shallow breathing
- Dizziness and/or nausea
- Reduced or lack of appetite
- Changes in sleep patterns
- Difficulty speaking and/or mumbled speech
It’s possible to move between hyper- and hypoarousal. Oftentimes, being in hyperarousal for an extended period of time can send the body into hypoarousal, and it’s common to return to a window of tolerance from one state and then enter into the other state when stressed or triggered again.
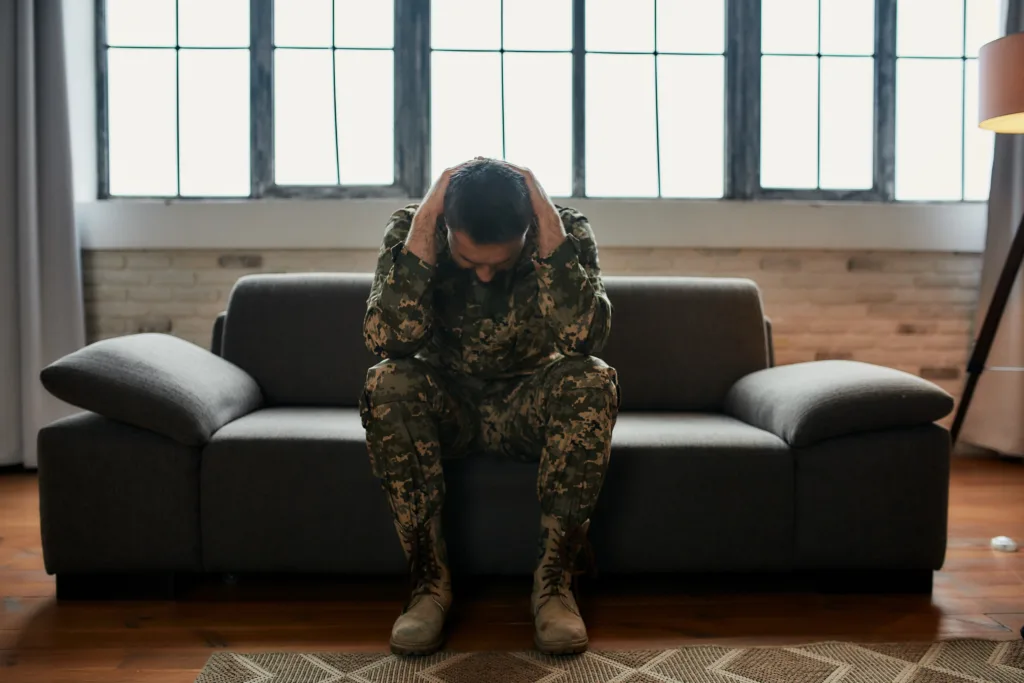
The Window of Tolerance and Veterans
Veterans returning to civilian life post-service with trauma symptoms or post-traumatic stress disorder (PTSD) often have a smaller capacity for flexibility and enduring stressful situations. According to Veterans Affairs, an average of 13.5% of veterans who served in Operation Enduring Freedom and Operation Iraqi Freedom exhibit PTSD symptoms. Experiencing or witnessing a traumatic event (or several smaller ones), such as combat, sexual assault or experiencing a moral injury can send someone into a state of hyper- or hypoarousal.
Without treatment, trauma can make daily living feel overwhelming because of a compromised and narrow window of tolerance, which can lead to harmful coping mechanisms, such as isolation and substance use. When veterans seek professional treatment and support, they receive education and guidance on how to observe their own unique triggers and responses, how to navigate and process stressful situations, and how to reconnect to their bodies to restore a sense of safety. These processes broaden the window of tolerance, allowing veterans to explore their social engagement system and experience joy in their relationships again.
It’s important to note that an activated nervous system or being out of a window of tolerance is not “wrong”. This is the body’s attempt to survive and find safety during and after extraordinary situations outside of what can be considered normal human experience.
How Pyramid Military Therapy & Recovery Programs Can Help
The curriculum at Pyramid Military Therapy & Recovery Programs is trauma-informed and uses a variety of evidence-based treatment modalities, such as cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT) and acceptance and commitment therapy (ACT). These are supported by the implementation of polyvagal theory, peer support and holistic and experiential therapies to treat the whole person.
Contact us or call 814-631-5676 to learn more.